Pregnancy, with its myriad wonders and complexities, is a transformative journey that brings both joy and challenges. At the heart of this remarkable experience lies the hormone progesterone, a silent orchestrator crucial for nurturing the delicate dance of life within. As expectant mothers embark on this extraordinary odyssey, understanding the profound role of progesterone becomes not just insightful but paramount for ensuring a healthy and flourishing pregnancy.
Progesterone, a naturally occurring hormone produced by the ovaries post-ovulation, takes center stage in preparing the uterine lining for potential pregnancy. Beyond its foundational role in creating a receptive environment for a fertilized egg, progesterone continues to be a steadfast guardian during the early stages of gestation. It plays a pivotal role in preventing uterine contractions that could lead to miscarriage and supports the development of the placenta, a lifeline for the growing fetus. In this exploration, we delve into the significance of maintaining optimal progesterone levels, the potential complications arising from deficiencies, and proactive measures that pave the way for a smoother and healthier pregnancy journey. Welcome to the unraveling journey of progesterone in pregnancy, where knowledge becomes a guiding light for expectant mothers navigating the intricacies of maternal well-being and fetal development.
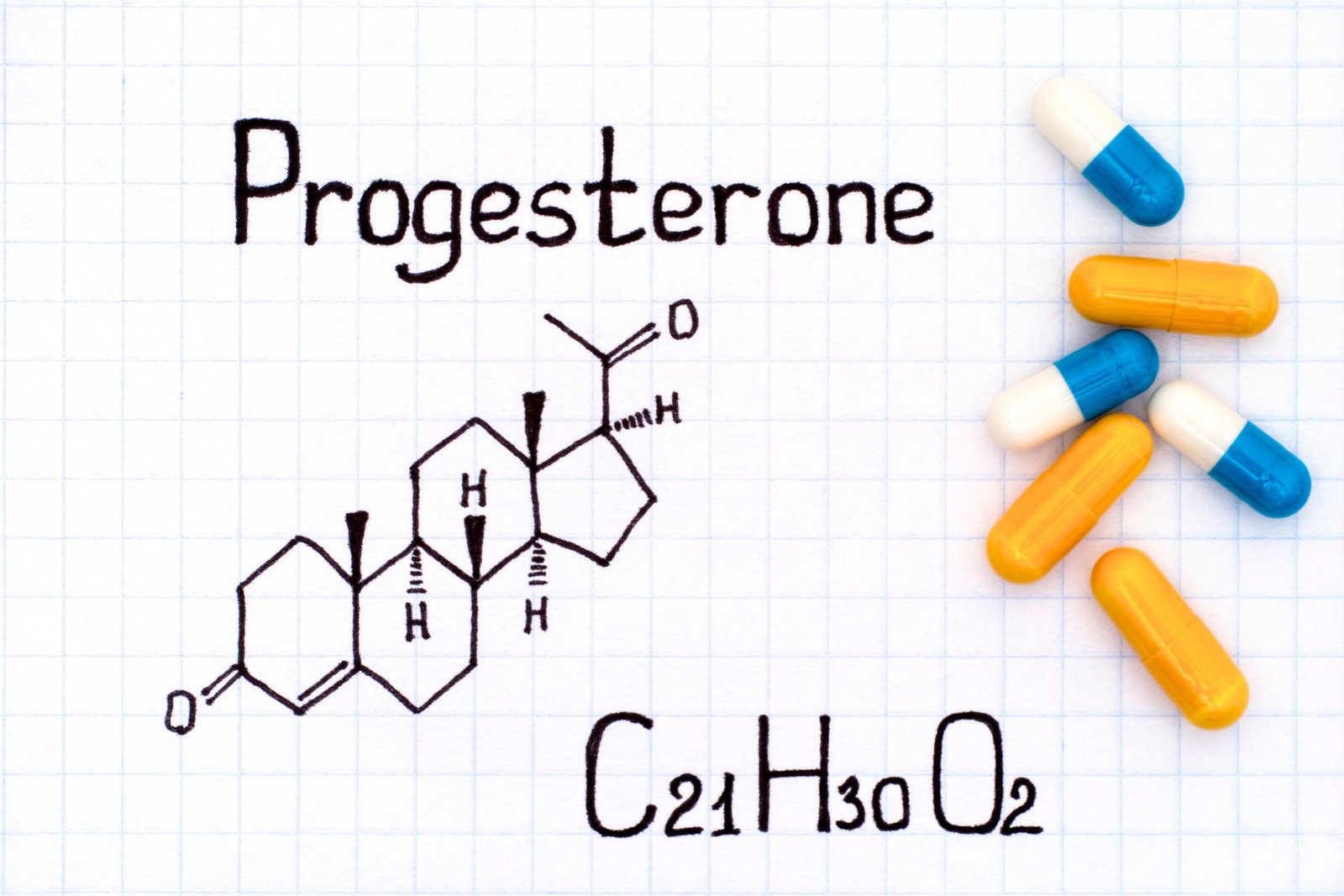
What is Progesterone?

Progesterone, an integral hormone in the realm of reproductive health, is a naturally occurring steroid hormone produced primarily by the ovaries post-ovulation. This essential component of the female reproductive system orchestrates a series of intricate processes that are vital for a successful pregnancy.
Uterine Lining Preparation
One of progesterone’s primary roles is to prepare the uterine lining, a crucial step in creating an optimal environment for a potential pregnancy. After ovulation, the hormone stimulates the thickening of the uterine lining, ensuring it becomes lush and receptive to the implantation of a fertilized egg.
Supportive Environment for Implantation
Progesterone takes center stage in creating a nurturing space for the fertilized egg to thrive. It prompts the uterine muscles to relax, preventing contractions that could disrupt the implantation process. This relaxation is instrumental in providing a stable foundation for the fertilized egg to embed itself securely in the uterine lining.
Sustaining Early Pregnancy
As pregnancy progresses, progesterone continues to play a pivotal role in supporting the developing embryo. It aids in the formation and maintenance of the placenta, a vital organ that facilitates the exchange of nutrients and waste between the mother and the growing fetus.
Understanding the multifaceted contributions of progesterone during early pregnancy is essential for appreciating its significance in ensuring a healthy and successful reproductive journey. From the initial preparation of the uterine lining to the continued support of the developing pregnancy, progesterone’s orchestration is nothing short of remarkable.
The Importance of Adequate Progesterone Levels

As pregnancy unfolds, the role of progesterone extends beyond its initial involvement in preparing the uterine lining. Adequate levels of this crucial hormone during the early stages of pregnancy are paramount for several pivotal reasons, ensuring a harmonious and healthy gestational period.
Prevention of Uterine Contractions
Progesterone acts as a natural safeguard against untimely uterine contractions, a phenomenon that could pose a significant threat to the developing pregnancy. By inducing a state of uterine muscle relaxation, progesterone helps thwart contractions that might otherwise jeopardize the implantation of the fertilized egg or lead to premature labor. This protective mechanism becomes particularly critical during the delicate early weeks of pregnancy.
Sustaining the Placental Development
As pregnancy progresses, progesterone plays a key role in supporting the development and maintenance of the placenta. The placenta serves as a lifeline, facilitating the exchange of nutrients, oxygen, and waste products between the mother and the growing fetus. Progesterone’s influence on placental formation ensures that this vital organ functions optimally, providing the necessary nourishment and support essential for the healthy growth and development of the unborn child.
Nurturing a Healthy Pregnancy
Progesterone’s dual role in preventing uterine contractions and promoting placental development contributes significantly to the overall health and sustainability of the pregnancy. Its presence is foundational in creating a stable and nurturing environment that fosters the well-being of both the mother and the developing fetus.
Understanding the pivotal contributions of progesterone during the early stages of pregnancy underscores the importance of maintaining optimal hormone levels. The delicate balance orchestrated by progesterone is a key determinant in ensuring a smooth and successful gestational journey.
When Progesterone Levels Fall Short

While progesterone plays a crucial role in supporting a healthy pregnancy, a deficiency in its levels can pose significant challenges and potential risks. Recognizing the signs of low progesterone and addressing the issue promptly is paramount for ensuring the well-being of both the expectant mother and the developing fetus.
Risks and Complications
Low progesterone levels during pregnancy raise concerns as they are associated with an increased risk of complications. The two primary complications linked to insufficient progesterone are miscarriage and preterm birth. Understanding the potential consequences underscores the urgency of addressing low progesterone levels to mitigate these risks.
Signs of Low Progesterone
Identifying the signs of low progesterone is crucial for timely intervention. Common indicators include:
Spotting or Vaginal Bleeding: Any unexplained bleeding during pregnancy warrants attention and investigation.
Abdominal Pain or Cramping: Persistent pain or cramping may signal a potential issue with hormonal balance.
Recurrent Miscarriages: A history of recurrent miscarriages may prompt healthcare providers to assess progesterone levels.
Diagnostic Measures
If there are concerns about progesterone levels, healthcare providers may employ various diagnostic measures, including blood tests, to assess hormone levels accurately. Monitoring progesterone levels during the early stages of pregnancy is particularly crucial, as this is when the hormone’s role in supporting implantation and preventing miscarriage is most pronounced.
Addressing Low Progesterone
If low progesterone levels are confirmed, medical intervention becomes essential. Treatment options may include:
Progesterone Supplementation: Hormone supplements, administered orally or through injections, can help raise and maintain progesterone levels.
Close Monitoring: Increased monitoring throughout the pregnancy, including more frequent ultrasounds and hormone level checks, may be recommended.
The Role of Personalized Care
Every pregnancy is unique, and addressing low progesterone levels requires personalized care. Collaborating closely with healthcare providers ensures a tailored approach that considers the specific needs and circumstances of each expectant mother.
In conclusion, recognizing the signs of low progesterone and taking prompt action is crucial in safeguarding the health and well-being of both mother and baby during pregnancy. Regular communication with healthcare professionals and adherence to recommended monitoring protocols contribute to a positive outcome for pregnancies affected by progesterone deficiency.
Reasons for Low Progesterone Levels

Several factors can contribute to a drop in progesterone levels, including:
Luteal Phase Defect: Unraveling the Impact on Progesterone Production

In the intricate world of reproductive health, the luteal phase holds a critical role in the menstrual cycle, influencing the delicate balance of hormones that regulate fertility. A luteal phase defect, characterized by a shortened second half of the menstrual cycle, can have profound implications, particularly in the context of progesterone production and its impact on the journey to conception.
Understanding the Luteal Phase
The menstrual cycle consists of two main phases: the follicular phase, dominated by the maturation of an egg within the ovary, and the luteal phase, which follows ovulation. The luteal phase is orchestrated by the corpus luteum, a temporary structure formed from the remnants of the ovarian follicle after ovulation. This phase is crucial for preparing the uterine lining for a potential pregnancy.
Luteal Phase Defect and Insufficient Progesterone
A luteal phase defect occurs when the second half of the menstrual cycle is shorter than the typical 12-14 days. This truncation can compromise the ability of the corpus luteum to produce an adequate amount of progesterone. Progesterone, which is crucial for the preparation and maintenance of the uterine lining, may fall short, impacting the chances of successful implantation and the early stages of pregnancy.
Signs and Symptoms
Women experiencing a luteal phase defect may observe certain signs and symptoms, including:
Shortened Menstrual Cycle: A luteal phase defect often manifests as a shortened time between ovulation and the start of menstruation.
Spotting Before Period: Light bleeding or spotting before the expected period may be indicative of insufficient progesterone levels.
Difficulty in Sustaining Pregnancy: Recurrent miscarriages or challenges in sustaining a pregnancy could be linked to a luteal phase defect.
Diagnosis and Treatment
Healthcare providers can diagnose a luteal phase defect through a combination of cycle tracking, hormonal assessments, and sometimes, imaging studies. Treatment options may include:
Progesterone Supplementation: Administering supplemental progesterone can compensate for the deficit and support a more favorable environment for pregnancy.
Lifestyle Modifications: Certain lifestyle changes, such as stress management and a balanced diet, may positively impact hormonal balance.
Fertility Considerations
For women trying to conceive, addressing a luteal phase defect is integral to optimizing fertility. Timely diagnosis and intervention can enhance the chances of successful conception and a healthy pregnancy.
In essence, understanding the intricate interplay between the luteal phase and progesterone production sheds light on potential challenges in the fertility journey. Recognizing and addressing a luteal phase defect is a crucial step toward fostering optimal reproductive health and increasing the likelihood of a successful pregnancy.
Ovarian Dysfunction: Unraveling the Impact on Progesterone Production

Within the delicate ballet of reproductive health, the ovaries play a starring role, orchestrating the hormonal symphony necessary for fertility and pregnancy. When these vital organs face dysfunction, it can have far-reaching consequences, particularly concerning the production of progesterone—a hormone integral to the success of conception and a healthy pregnancy.
The Ovaries’ Role in Hormonal Harmony
The ovaries, a pair of small, almond-shaped organs, are pivotal in the female reproductive system. Their primary functions include the release of eggs (ovulation) and the production of hormones, including estrogen and progesterone. Progesterone, in particular, is crucial for preparing the uterine lining and sustaining a conducive environment for a potential pregnancy.
Impact of Ovarian Dysfunction on Progesterone
Ovarian dysfunction encompasses various conditions that can disrupt the normal functioning of the ovaries. This dysfunction can directly impact the ovaries’ ability to produce an adequate amount of progesterone. Conditions such as polycystic ovary syndrome (PCOS), ovarian cysts, or premature ovarian failure can disrupt the intricate hormonal balance necessary for reproductive health.
Polycystic Ovary Syndrome (PCOS)
PCOS, a common hormonal disorder among women of reproductive age, often leads to irregular ovulation or anovulation. In the absence of regular ovulation, the corpus luteum—a temporary structure formed after ovulation that produces progesterone—may not develop adequately, resulting in lower progesterone levels. This imbalance can hinder the preparation of the uterine lining and increase the risk of miscarriage.
Ovarian Cysts
The presence of ovarian cysts, fluid-filled sacs on or within the ovaries, can also impact progesterone production. Cysts may interfere with the normal ovulatory process, reducing the formation of the corpus luteum and, consequently, the production of progesterone.
Premature Ovarian Failure
Premature ovarian failure, a condition where the ovaries cease normal function before the age of 40, can significantly disrupt hormonal balance. The resulting decline in progesterone production can compromise the ability to sustain a pregnancy.
Diagnostic Measures and Treatment
Healthcare providers employ various diagnostic measures, including hormonal assessments and imaging studies, to identify ovarian dysfunction. Treatment options may include:
Hormone Therapy: In some cases, hormone therapy may be prescribed to regulate hormonal levels, including progesterone.
Fertility Treatments: For those trying to conceive, assisted reproductive technologies may be considered to overcome ovulatory challenges.
Fostering Reproductive Health
Addressing ovarian dysfunction requires a personalized approach, taking into account the specific conditions affecting the ovaries. Collaborating closely with healthcare professionals ensures tailored interventions that can optimize reproductive health and increase the chances of a successful pregnancy.
In conclusion, recognizing the impact of ovarian dysfunction on progesterone production emphasizes the importance of proactive management and targeted treatments. A comprehensive understanding of these interconnections is crucial for individuals navigating fertility challenges and seeking a pathway to a healthy and fulfilling reproductive journey.
Stress and Hormonal Balance: Navigating the Impact on Progesterone Production

In the intricate landscape of reproductive health, stress emerges as a powerful player that can influence hormonal harmony, potentially affecting fertility and the successful progression of pregnancy. Understanding the dynamic relationship between stress and progesterone production unveils a critical aspect of the broader journey toward conception and a healthy gestation.
The Stress-Hormone Connection
Stress triggers a complex cascade of physiological responses, including the release of stress hormones like cortisol. This hormonal surge, designed for immediate response to perceived threats, can inadvertently interfere with the delicate balance of reproductive hormones, including progesterone.
Stress and Ovulation
Elevated stress levels have been associated with disruptions in the normal ovulatory process. Stress-induced hormonal fluctuations can impact the release of luteinizing hormone (LH), a key regulator of ovulation. Irregular ovulation can subsequently lead to inadequate development of the corpus luteum—the structure responsible for progesterone production.
Progesterone Suppression
Chronic stress may contribute to the suppression of progesterone production. As the stress response prioritizes immediate survival needs over reproductive functions, the body may allocate resources away from maintaining the corpus luteum, resulting in decreased progesterone levels. This hormonal imbalance can compromise the preparation of the uterine lining and increase the risk of difficulties in conceiving or sustaining a pregnancy.
Impact on Menstrual Cycle
Stress can manifest in various ways, affecting the menstrual cycle in different individuals. Some may experience irregular cycles, while others may encounter changes in the duration and intensity of menstruation. These variations can reflect disruptions in hormonal balance, including progesterone fluctuations.
Coping Mechanisms and Lifestyle Changes
Recognizing the link between stress and hormonal imbalance highlights the importance of adopting effective coping mechanisms. Strategies to manage stress may include:
Mind-Body Techniques: Practices such as mindfulness, meditation, and yoga can help alleviate stress and promote overall well-being.
Balanced Lifestyle: Prioritizing a healthy lifestyle, including regular exercise, sufficient sleep, and a balanced diet, contributes to resilience against stress-induced hormonal disruptions.
Seeking Professional Support
For individuals navigating infertility or challenges in sustaining a pregnancy, seeking support from healthcare professionals is crucial. Fertility specialists and mental health professionals can collaborate to develop tailored strategies that address both the physiological and psychological aspects of stress-related fertility concerns.
Holistic Approaches to Fertility
Taking a holistic approach to reproductive health involves acknowledging the interconnectedness of physical and emotional well-being. Managing stress becomes an integral part of optimizing fertility and supporting a healthy pregnancy journey.
In conclusion, understanding the impact of stress on hormonal balance, including progesterone production, emphasizes the significance of comprehensive care. Integrating stress management into fertility strategies not only enhances the chances of conception but also contributes to overall reproductive well-being.
Certain Medications and Their Impact on Progesterone Levels

In the intricate landscape of reproductive health, medications play a significant role, offering solutions to various health issues. However, it’s essential to recognize that some medications may influence hormonal balance, including the levels of progesterone. Understanding the potential impact of certain drugs on progesterone production is crucial for individuals navigating fertility concerns or aiming for a healthy pregnancy.
Hormonal Disruption by Medications
Certain medications, while addressing specific health conditions, can inadvertently interfere with the delicate equilibrium of reproductive hormones. This disruption can extend to progesterone, a key player in the preparation of the uterine lining and the maintenance of a conducive environment for pregnancy.
Types of Medications that Affect Progesterone
Hormonal Birth Control: While hormonal contraceptives are designed to regulate the menstrual cycle and prevent ovulation, their cessation can sometimes lead to a temporary delay in the resumption of normal ovulatory function. This delay can impact progesterone production and the subsequent preparation of the uterine lining.
Certain Anti-Inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs), if used regularly and in high doses, may interfere with ovulation and progesterone synthesis. It’s important to use these medications as directed and consult healthcare providers if concerns arise.
Corticosteroids: Medications such as corticosteroids, commonly used to manage inflammatory conditions, can potentially impact the normal functioning of the ovaries and hormonal balance.
Implications for Fertility
For individuals trying to conceive, understanding the potential impact of medications on progesterone levels is crucial. Disruptions in the normal hormonal milieu can affect the timing and success of ovulation, potentially influencing the chances of conception.
Communication with Healthcare Providers
Open and transparent communication with healthcare providers is paramount, especially for individuals planning a pregnancy or facing fertility challenges. Disclosing all medications, including over-the-counter and prescription drugs, allows healthcare providers to make informed decisions regarding fertility interventions.
Individualized Approaches
Recognizing that the impact of medications on progesterone levels can vary among individuals underscores the importance of personalized care. Healthcare providers may tailor treatment plans based on an individual’s specific health condition, medication history, and reproductive goals.
Lifestyle Considerations
In addition to medication management, adopting a healthy lifestyle contributes to overall reproductive well-being. A balanced diet, regular exercise, and stress management play integral roles in supporting hormonal balance and fertility.
Seeking Specialist Advice
For those facing fertility challenges related to medication use, seeking guidance from fertility specialists is crucial. These experts can provide targeted interventions and advice on navigating the complexities of medication-related hormonal disruptions.
In conclusion, while medications can be invaluable for managing health conditions, awareness of their potential impact on progesterone levels is vital for those with fertility aspirations. Collaborating closely with healthcare providers ensures a holistic approach to reproductive health that encompasses both medication management and lifestyle considerations.
What to Do if Progesterone is Too Low

If low progesterone is detected, medical intervention may be necessary. Options include:
Progesterone Supplementation: Nurturing Pregnancy with Hormonal Support
When facing challenges associated with low progesterone levels during pregnancy, healthcare providers may turn to a solution known as progesterone supplementation. This therapeutic approach involves the administration of hormone supplements to elevate and sustain progesterone levels, fostering a supportive environment for a healthy and successful pregnancy.
Purpose of Progesterone Supplementation
Progesterone supplementation is primarily employed to address situations where the body’s natural production of progesterone may be insufficient. This intervention becomes particularly crucial when low progesterone levels pose a risk to the viability of the pregnancy, increasing the likelihood of complications such as miscarriage.
Forms of Progesterone Supplements
Progesterone supplements are available in various forms, allowing healthcare providers to tailor the treatment to the specific needs and circumstances of the expectant mother. Common forms of progesterone supplementation include:
Oral Progesterone: Administered in pill form, oral progesterone is convenient and easily managed. However, it undergoes metabolism in the liver, which can result in lower bioavailability.
Vaginal Progesterone: Suppositories or gels applied directly into the vagina offer a localized delivery method, enhancing the absorption of progesterone and providing a more targeted impact on the uterine lining.
Intramuscular Progesterone: Injected into the muscle, intramuscular progesterone provides a sustained release of the hormone. This method is often used in situations where consistent, elevated progesterone levels are crucial.
Timing and Duration of Supplementation
The timing and duration of progesterone supplementation depend on the unique circumstances of each pregnancy. Healthcare providers may recommend supplementation during specific phases, such as the early weeks when the risk of miscarriage is higher, or throughout the entire first trimester. The duration is often guided by ongoing assessments of progesterone levels and the progression of the pregnancy.
Monitoring and Adjustments
Regular monitoring of progesterone levels is a key aspect of supplementation. Healthcare providers conduct blood tests to assess the effectiveness of the intervention and may adjust the dosage or form of supplementation as needed to maintain optimal progesterone levels.
Progesterone Supplementation in Assisted Reproductive Technologies (ART)
For individuals undergoing assisted reproductive technologies, such as in vitro fertilization (IVF), progesterone supplementation is commonly employed to support the implantation of embryos and sustain early pregnancy. This is often initiated shortly after the embryo transfer and continues until the placenta takes over progesterone production.
Considerations and Side Effects
While progesterone supplementation is generally considered safe, it may be associated with side effects such as drowsiness, breast tenderness, or irritation at the application site. As with any medical intervention, potential risks and benefits are carefully weighed, and healthcare providers work collaboratively with patients to ensure informed decision-making.
The Holistic Approach to Hormonal Support
Progesterone supplementation is one aspect of a holistic approach to managing hormonal imbalances during pregnancy. It is often complemented by lifestyle adjustments, nutritional considerations, and ongoing medical support to optimize the chances of a healthy and successful pregnancy.
In conclusion, progesterone supplementation stands as a valuable tool in the arsenal of interventions aimed at nurturing pregnancies facing challenges related to progesterone levels. Its judicious use, guided by thorough monitoring and individualized care, contributes to the realization of healthy pregnancies and the joy of welcoming a new life into the world.
Lifestyle Changes: Cultivating Hormonal Harmony for a Healthy Pregnancy

Embarking on the journey of pregnancy involves more than medical interventions; lifestyle choices play a pivotal role in fostering optimal hormonal balance. Managing stress, adopting a nutritious diet, and incorporating regular exercise into daily life are proactive measures that can positively impact hormonal equilibrium, enhancing the chances of a healthy and successful pregnancy.
Stress Management for Hormonal Balance
Chronic stress can disrupt the delicate interplay of hormones, including progesterone, essential for a healthy pregnancy. Incorporating stress management techniques into daily routines is vital. Consider:
Mindfulness and Meditation: Practices that promote mindfulness and meditation can help reduce stress levels, allowing the body to maintain hormonal balance.
Breathing Exercises: Deep-breathing exercises, such as diaphragmatic breathing, offer a simple yet effective way to alleviate stress and support overall well-being.
Yoga: The combination of gentle movement, stretching, and mindfulness in yoga can contribute to stress reduction and hormonal harmony.
Nutrient-Rich Diet for Hormonal Health
A well-balanced and nutritious diet provides the foundation for hormonal health during pregnancy. Key considerations include:
Folate and Vitamin B-Rich Foods: These nutrients are crucial for early fetal development. Incorporate leafy greens, legumes, and fortified grains into your diet.
Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, omega-3 fatty acids support brain and vision development in the fetus.
Lean Proteins: Sources such as poultry, fish, and plant-based proteins contribute to overall health and provide essential amino acids.
Whole Grains: Opt for whole grains like brown rice, quinoa, and oats for fiber and sustained energy.
Hydration: Staying well-hydrated supports bodily functions, including hormonal balance. Water is an excellent choice for hydration.
Regular Exercise to Support Hormonal Well-Being
Physical activity is a cornerstone of a healthy lifestyle and can positively influence hormonal balance. Tailor your exercise routine to your fitness level and consult with healthcare providers if needed. Consider:
Aerobic Exercise: Activities like brisk walking, swimming, or cycling contribute to cardiovascular health and overall well-being.
Strength Training: Building and maintaining muscle mass through strength training exercises support metabolic health and can enhance fertility.
Yoga and Pilates: These practices not only improve flexibility and strength but also promote relaxation and stress reduction.
Pelvic Floor Exercises: Strengthening the pelvic floor muscles can be beneficial for both prenatal and postnatal well-being.
Holistic Approaches to Wellness
Incorporating holistic approaches into daily life enhances the potential for a healthy pregnancy. Consider:
Adequate Sleep: Prioritize sufficient and quality sleep to support overall physical and mental health.
Limiting Caffeine and Alcohol: Moderation in caffeine and alcohol consumption aligns with recommendations for a healthy pregnancy.
Avoiding Tobacco and Illicit Drugs: Steering clear of these substances is crucial for fetal development and maternal health.
Consultation with Healthcare Providers
Before making significant lifestyle changes during pregnancy, it’s essential to consult with healthcare providers. They can offer personalized guidance based on individual health conditions, ensuring that lifestyle adjustments align with the unique needs of each pregnancy.
Embracing a Wellness-Centric Pregnancy
In summary, adopting a lifestyle that prioritizes stress management, a nutritious diet, and regular exercise contributes to a wellness-centric pregnancy. These proactive measures not only support hormonal balance but also create a foundation for overall health, fostering an environment conducive to the joyous arrival of a new life.
Prevention is Key

While not all causes of low progesterone can be prevented, there are steps women can take to promote hormonal health:
Maintaining a Healthy Lifestyle: Nurturing Well-Being for a Flourishing Pregnancy

Cultivating a healthy lifestyle is more than a recommendation; it’s a cornerstone for promoting overall well-being, particularly during the transformative journey of pregnancy. A balanced diet and regular exercise stand as integral components, offering profound benefits that extend beyond individual health to positively influence the health of both the expectant mother and the growing fetus.
The Significance of a Balanced Diet
Nutrient-Rich Choices: Opting for a variety of nutrient-dense foods ensures a well-rounded intake of essential vitamins and minerals. Emphasize fruits, vegetables, whole grains, lean proteins, and dairy or dairy alternatives for a diverse nutrient profile.
Folate and Iron: Adequate folate is crucial in the early stages of pregnancy to prevent neural tube defects. Iron-rich foods support the increased blood volume and prevent anemia.
Calcium for Bone Health: Dairy products, leafy greens, and fortified alternatives provide essential calcium, supporting the development of the baby’s bones and teeth.
Hydration: Staying hydrated is fundamental for bodily functions, aiding digestion, nutrient transportation, and temperature regulation. Water is the best choice for hydration.
Moderation and Variety: A balanced diet embraces moderation and variety, avoiding excessive consumption of certain foods while incorporating a diverse range of nutrients.
The Role of Regular Exercise
Cardiovascular Health: Engaging in aerobic activities such as brisk walking, swimming, or low-impact aerobics supports cardiovascular health, contributing to overall fitness.
Strength and Flexibility: Incorporating strength training exercises helps maintain muscle tone and supports the body’s changing needs during pregnancy. Flexibility exercises, like stretching or yoga, enhance joint mobility.
Pelvic Floor Exercises: Strengthening the pelvic floor muscles can be particularly beneficial, offering support during pregnancy and helping in postnatal recovery.
Weight Management: Regular exercise, paired with a balanced diet, contributes to healthy weight management during pregnancy. Maintaining a healthy weight is associated with better maternal and fetal outcomes.
Mental Well-Being: Exercise is not only beneficial for physical health but also for mental well-being. It can help reduce stress, improve mood, and promote better sleep.
Integrating Lifestyle Choices for Optimal Well-Being
Preconception Health: A healthy lifestyle is not only vital during pregnancy but also before conception. Preconception health sets the stage for a healthy pregnancy and can positively impact fertility.
Regular Prenatal Check-ups: Consulting with healthcare providers throughout pregnancy ensures that lifestyle choices align with the specific needs of each expectant mother. Healthcare providers can offer guidance on nutrition, exercise, and overall wellness.
Adaptations for Individual Needs: Every pregnancy is unique, and lifestyle choices may need to be adapted based on individual health conditions, preferences, and the guidance of healthcare providers.
Hygiene Practices: In addition to diet and exercise, maintaining good hygiene practices is essential for overall health. This includes proper dental care, handwashing, and adherence to hygiene recommendations provided by healthcare professionals.
Embracing a Holistic Approach
In essence, maintaining a healthy lifestyle during pregnancy involves embracing a holistic approach that considers physical, mental, and emotional well-being. A balanced diet and regular exercise form the bedrock of this approach, fostering an environment conducive to a flourishing pregnancy and the well-being of both mother and child.
Managing Stress: Elevating Pregnancy Well-Being through Mindful Practices

Amidst the joy and anticipation of pregnancy, managing stress becomes a crucial component of fostering a positive and nurturing environment. Incorporating stress-reducing practices into daily life can not only enhance the well-being of the expectant mother but also contribute to a healthier pregnancy journey. Mindful practices, such as meditation and yoga, offer effective tools for stress management, providing both physical and mental benefits.
The Impact of Stress on Pregnancy
Hormonal Balance: Chronic stress triggers the release of stress hormones like cortisol, potentially disrupting the delicate hormonal balance required for a healthy pregnancy.
Fetal Development: Prolonged stress may influence fetal development and increase the risk of complications, emphasizing the importance of stress management for the well-being of both mother and baby.
Maternal Well-Being: Stress can contribute to fatigue, mood swings, and sleep disturbances, highlighting the need for effective stress-reducing strategies during pregnancy.
Meditation for Mindful Tranquility
Mindfulness Meditation: Incorporating mindfulness meditation involves cultivating a heightened awareness of the present moment. This practice encourages staying present without judgment, fostering a sense of calm and reducing anxiety.
Deep Breathing Techniques: Simple yet powerful, deep breathing exercises calm the nervous system, helping to alleviate stress. Techniques such as diaphragmatic breathing or guided breathing meditations can be easily integrated into daily routines.
Guided Imagery: Visualization techniques, where expectant mothers imagine peaceful and positive scenes, can contribute to relaxation and stress reduction.
Body Scan Meditation: This involves directing focused attention to different parts of the body, promoting relaxation and releasing tension.
Yoga for Physical and Mental Harmony
Gentle Prenatal Yoga: Tailored specifically for pregnant individuals, prenatal yoga incorporates gentle poses, stretches, and breathing exercises. It supports physical flexibility, relaxation, and a connection with the body.
Mindful Movement: Engaging in yoga fosters mindful movement, allowing individuals to connect with their bodies and the changes occurring during pregnancy.
Stress-Reducing Asanas: Certain yoga poses, such as child’s pose, cat-cow stretch, and legs-up-the-wall pose, are known for their stress-reducing benefits. These poses can be adapted for the comfort and safety of pregnant individuals.
Community and Support: Participating in prenatal yoga classes provides a supportive community where expectant mothers can share experiences, concerns, and coping strategies.
Integrating Mindfulness into Daily Life
Consistency is Key: Incorporating mindfulness practices into daily life requires consistency. Establishing a routine, even if brief, promotes the cumulative benefits of these practices.
Mindful Eating: Applying mindfulness to eating habits by savoring each bite and paying attention to hunger and fullness cues contributes to a holistic approach to well-being.
Mindful Communication: Nurturing positive relationships and effective communication with partners, family, and friends is integral to managing stress during pregnancy.
Seeking Professional Guidance
While mindfulness practices can be immensely beneficial, it’s essential to consult healthcare providers, especially if there are underlying health conditions or concerns. They can offer personalized advice and ensure that chosen practices align with the specific needs of each pregnancy.
In conclusion, integrating stress-reducing practices such as meditation and yoga into daily life is a proactive and empowering approach to pregnancy well-being. These mindful tools not only alleviate stress but also foster a sense of tranquility, contributing to a positive and harmonious pregnancy journey.
Regular Check-ups: Nurturing Pregnancy Health through Comprehensive Monitoring

The Importance of Regular Prenatal Check-ups
Hormonal Monitoring: Regular prenatal check-ups encompass monitoring key hormonal levels, including progesterone, estrogen, and human chorionic gonadotropin (hCG). These hormones play pivotal roles in sustaining a healthy pregnancy.
Fetal Development Assessment: Through various diagnostic measures such as ultrasounds and blood tests, healthcare providers can assess the growth and development of the fetus, ensuring it aligns with established milestones.
Blood Pressure and Glucose Checks: Monitoring blood pressure and glucose levels is crucial for identifying and managing conditions such as gestational hypertension and gestational diabetes, which can impact both maternal and fetal well-being.
Detection of Complications: Regular check-ups enable the early detection and management of potential complications, such as preeclampsia or placental issues, minimizing risks to both mother and baby.
Maternal Health Assessment: Evaluating the overall health of the expectant mother, including physical and emotional well-being, allows healthcare providers to tailor care plans and support optimal pregnancy outcomes.
Hormonal Monitoring during Pregnancy
Progesterone Levels: Regular prenatal visits involve monitoring progesterone levels, especially in the early stages of pregnancy. Adequate progesterone is vital for maintaining the uterine lining and preventing miscarriage.
Estrogen Levels: Estrogen, another essential hormone during pregnancy, contributes to the growth and development of the fetus and the maintenance of the placenta.
hCG Levels: Human chorionic gonadotropin (hCG) levels are routinely assessed, providing insights into the health of the developing pregnancy. Deviations from expected hCG patterns may indicate potential issues.
Frequency of Prenatal Check-ups
First Trimester: Prenatal check-ups during the first trimester may be more frequent, allowing healthcare providers to closely monitor early pregnancy developments, including hormonal changes.
Second and Third Trimesters: As the pregnancy progresses, the frequency of check-ups may reduce but remains regular to ensure ongoing monitoring and timely intervention if needed.
Active Communication with Healthcare Providers
Open Dialogue: Establishing open communication with healthcare providers is essential. Expectant mothers should feel empowered to discuss any concerns, changes in symptoms, or emotional well-being during these visits.
Collaborative Decision-Making: Prenatal check-ups offer opportunities for collaborative decision-making. Healthcare providers and expectant mothers work together to make informed choices about various aspects of care, including hormonal monitoring.
Beyond Hormonal Monitoring
Ultrasound Examinations: Regular ultrasounds provide visual assessments of fetal development, ensuring that growth is on track and identifying any structural abnormalities.
Screening Tests: Various screening tests, such as genetic screenings and non-invasive prenatal testing (NIPT), may be offered during prenatal check-ups to assess the risk of certain conditions.
Personalized Care Plans
Tailored Interventions: Regular check-ups allow healthcare providers to tailor interventions based on the unique needs and circumstances of each pregnancy. This individualized approach supports the health and well-being of both mother and baby.
Educational Opportunities: Prenatal visits serve as educational opportunities, providing expectant parents with information on pregnancy, childbirth, and postpartum care.
Adapting to Changing Needs
High-Risk Pregnancies: For pregnancies deemed high-risk due to pre-existing conditions or emerging complications, more frequent and specialized monitoring may be recommended.
Telehealth Options: In some situations, telehealth options may be utilized for routine check-ups, providing convenience without compromising the quality of care.
Conclusion

In closing, the journey of pregnancy, intricately woven with the symphony of hormonal changes, finds its silent maestro in progesterone. This vital hormone, diligently produced by the ovaries, orchestrates the symphony of fetal development and maternal well-being. Through understanding its role and actively participating in its management, expectant mothers become architects of a harmonious and healthy pregnancy.
As we unveil the significance of progesterone, it becomes evident that regular monitoring, early identification of potential issues, and proactive interventions are the pillars of a resilient and flourishing pregnancy journey. The partnership between expectant mothers and healthcare providers, guided by knowledge and personalized care, paints a canvas where the delicate balance of hormones aligns with the rhythms of new life.
In this narrative of progesterone’s role in pregnancy, we celebrate not only the physiological marvels but also the empowerment that knowledge brings. Armed with insights, expectant mothers embark on a journey where each heartbeat, each milestone, is a testament to the collaborative dance between nature and nurture. As we conclude this exploration, we honor the resilience, wisdom, and unwavering strength that define the journey of pregnancy, where progesterone stands as a silent but powerful ally.
The information provided in this article is intended for general knowledge and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Every pregnancy is unique, and individual circumstances vary. Pregnant women are strongly encouraged to consult with their healthcare providers for personalized guidance on all aspects of their pregnancy journey, including emotional well-being, fitness activities, and any specific concerns they may have. Healthcare providers possess the expertise to offer tailored advice based on a thorough understanding of an individual’s health history and current pregnancy status.